At St. Catherine Specialty Hospital in Zagreb, Croatia, a new chapter in healthcare is unfolding: the combination of full-genome sequencing and sophisticated artificial intelligence tools is now being used in clinical practice even for healthy individuals seeking preventive insights. According to a recent report, the hospital “is among the first globally to implement whole genome sequencing in routine clinical practice”.
The hospital’s service, known as the Genome4All test, examines over 20,000 genes and sequences more than three billion bases of DNA, essentially the full genomic blueprint of a person.
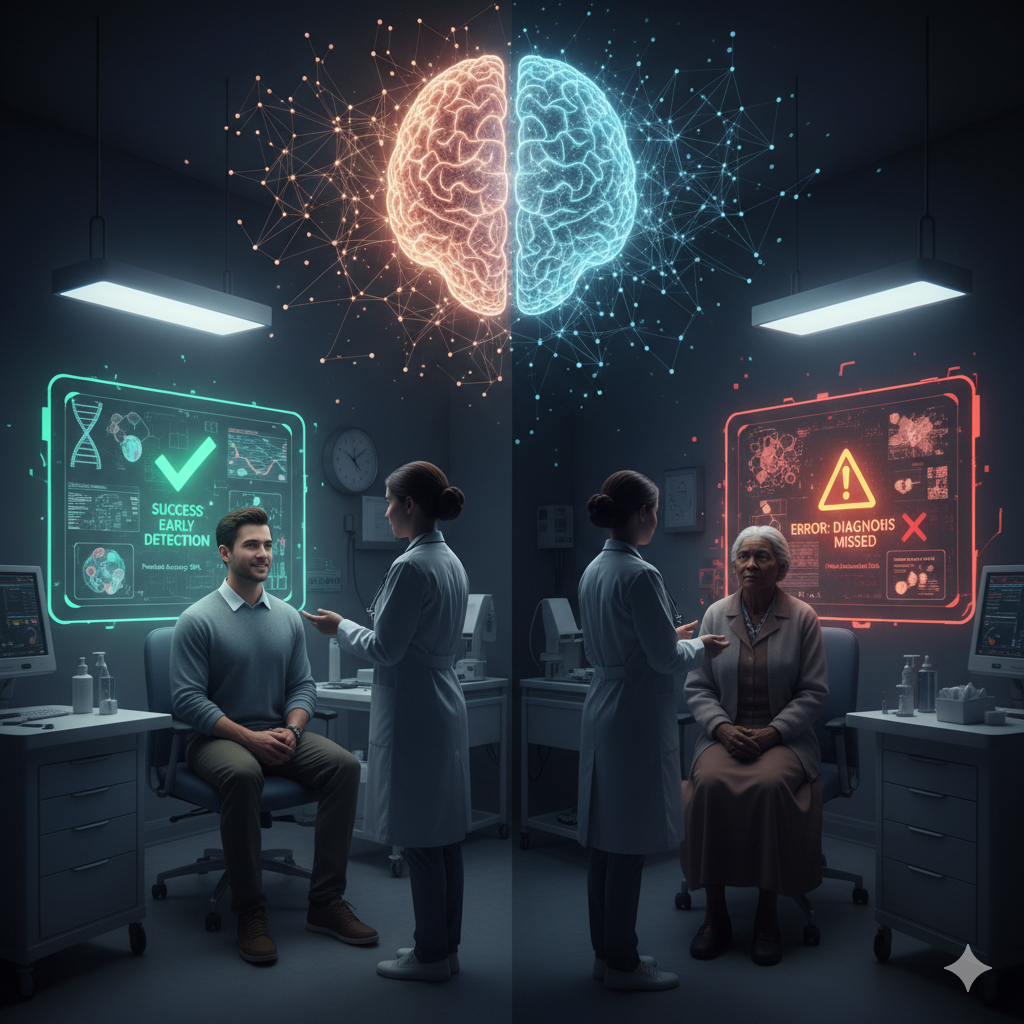
Once the blood sample is processed, powerful artificial intelligence algorithms take over. Because the volume of data is enormous, these algorithms sift through thousands of genetic variants, compare the patient’s genome to large reference databases, predict which variants are likely to cause disease, analyse tumour profiles in oncology cases and support clinical decision-making. As Dr Dragan Primorac observed: “the genome is a system of two billion letters, with each letter … being analysed using artificial intelligence”.
For example, in oncology, when a tumour’s origin is unknown, a tool developed by the hospital uses artificial intelligence trained on more than 20,000 tumour genomes to predict the most likely primary site, offering a pathway to better-targeted therapy.
Then, results are translated into clinical reports: risk of inherited disease (cancer, cardiovascular, metabolic), pharmacogenomic guidance (which drugs and doses might suit a patient), tumour origin in cancer of unknown primary, and so on.
By identifying inherited genetic risks early or aligning therapy to a person’s unique genome, outcomes can improve and healthcare resources may be spent more efficiently.
Key Barriers
Although full genome sequencing plus artificial intelligence is now in use, expanding this across the public hospital system will require significant investment in infrastructure, data systems and training.
Many detected variants still have unclear significance; AI helps, but human expertise remains essential.
Whole-genome data is personal and sensitive. Governance, consent and data protection frameworks must keep pace.
Conclusion
By sequencing entire genomes and using artificial intelligence to analyse the data, clinicians can spot disease risks earlier, choose treatments that are customized to each person, and make healthcare resources work better. Although there are still hurdles such as infrastructure, data complexity and privacy, this initiative shows that when technology, medicine and data join forces, we can deliver smarter and more effective care.
References
“Croatia at the frontier of personalized medicine” (EU Reporter) – describes WGS in routine practice at St. Catherine.
“Results of first whole genome sequencing in Croatia presented” (HINA News)
Genome4All test description (St. Catherine website)